Oxytocin versus Pitocin®: Induction of Labor in Different Worlds - Part 3 of 3
What would a world without love look like? This is where the controversy over oxytocin versus Pitocin® begins. And it’s unclear where it will end…
In Part 1 of this series, I focused on oxytocin and its activities throughout the pregnancy continuum. In Part 2 I focused on the increased use of synthetic oxytocin (Pitocin®) in the conventional, hospital-based maternity care mode. In this final part, I will be focusing on the potential detrimental effects of the nearly ubiquitous use of Pitocin® in U.S.-based childbirth, considering that 98% or more of birth are happening within hospitals.
Pitocin® ain’t oxytocin
In Part 1, I asked you earlier to consider: “What would a world without love look like?”
Before get around to answering that question, let’s revisit endogenous oxytocin, which is produced in the magnocellular neurons connecting the hypothalamus to the posterior pituitary, then released from the latter in a pulsatile fashion, influencing orgasm, ejaculation, conception, uterine contractions, and milk let-down. Vasopressin (ADH) is very similar in structure and produced and released in the same fashion.
Synthetic oxytocin (Pitocin®, Syntocin®) is infused in a continuous fashion for various reasons in the hospital, including induction of labor (IOL) and augmentation of labor (“speeding up” uterine contractions). It is also used commonly in out-of-hospital birth by reducing postpartum bleeding, though it’s usually given in a single intramuscular injection in this setting.
The most concerning risk of Pitocin® infusion is uterine tachysystole, defined as more than 5 uterine contractions over a 10-minute interval. Pitocin®, like its natural cousin, is also known to cause hypotension when infused continuously; however, due to its similarity in structure to ADH, the U.S. Food & Drug Administration (FDA) includes a warning regarding hypertension:
“…oxytocin even in its pure form has inherent pressor and antidiuretic properties which may become manifest when large doses are administered. These properties are thought to be due to the fact that oxytocin and vasopressin differ in regard to only two of the eight amino acids”
If you recall, vasopressin (ADH) boosts blood pressure by retaining water in the kidney nephron as well as through direct narrowing of blood vessels. This action is in the name itself: vaso- (vessel) + -pressin (pressure).
The retention of water certainly increases pressure within the pipes, but it also changes the molarity of your blood, meaning it becomes more dilute.
The beauty of natural oxytocin
The structures of oxytocin and Pitocin® are identical as far as I can tell. Fine.
But the imposter also includes a preservative in the form of 0.5% Chlorobutanol, a chloroform derivative. I don’t have much more to say about this except that we now no longer have two comparable chemicals, as Pitocin® has this other additive, which is not coupled with the real stuff released from the brain. What are the consequences of including this preservative? Who knows.
Let me wax poetic for a moment about endogenous oxytocin.
The beauty of oxytocin has been on my mind ever since I read the works of Michel Odent, MD, a retired French surgeon who has been advocating for natural childbirth for decades. If you’re curious about this man, I suggest starting with: “The Functions of the Orgasms: The Highways to Transcendence”. Mind. Blown.
As we have already discussed, oxytocin has a wide range of benefits to mothers and their babies. Men also benefit indirectly form their own oxytocin signaling in order to connect with their newborns and with their partners.
And if the reason that we fall in love with our partners, babies, and friends at least in part due to oxytocin’s influences on the brain and psyche, how do we measure love?
One thing I haven’t yet mentioned is that while oxytocin is released into the blood in a pulsatile fashion to exert its effects on the heart and uterus, it’s released in a continuous fashion in the brain to exert its effects on the brain. This means that oxytocin is both a hormone (blood) and neurotransmitter (nervous system).
If we pump women full of Pitocin® while in labor, are these same benefits seen?
Continuous infusion of Pitocin® is probably relevant
Sarah Buckley, MD, and her colleagues looked at oxytocin levels in the blood of laboring women. Their methods for doing this ranged from peripheral to jugular blood draws as well as cerebrospinal fluid (CSF) collection (no thank you)! They found that the frequency of the “pulses” and the amounts of oxytocin released from the pituitary occurred increased steadily throughout pregnancy in response to estrogen, and it rises rapidly throughout the stages of labor, reaching a 3-4-fold rise above baseline at the peak of childbirth. There was a separate spike associated with the 3rd stage (placental expulsion). Interesting, the pulsatile release of oxytocin didn’t necessarily correspond with the timing of uterine contractions. Oxytocin levels also rose within the CSF. Pitocin® is infused at a continuous rate in the hospital, and we aren’t sure that it crosses the blood brain barrier. Buckley’s research suggests that it does not at the low doses necessitated by a concern for tachysystole during continuous infusion.
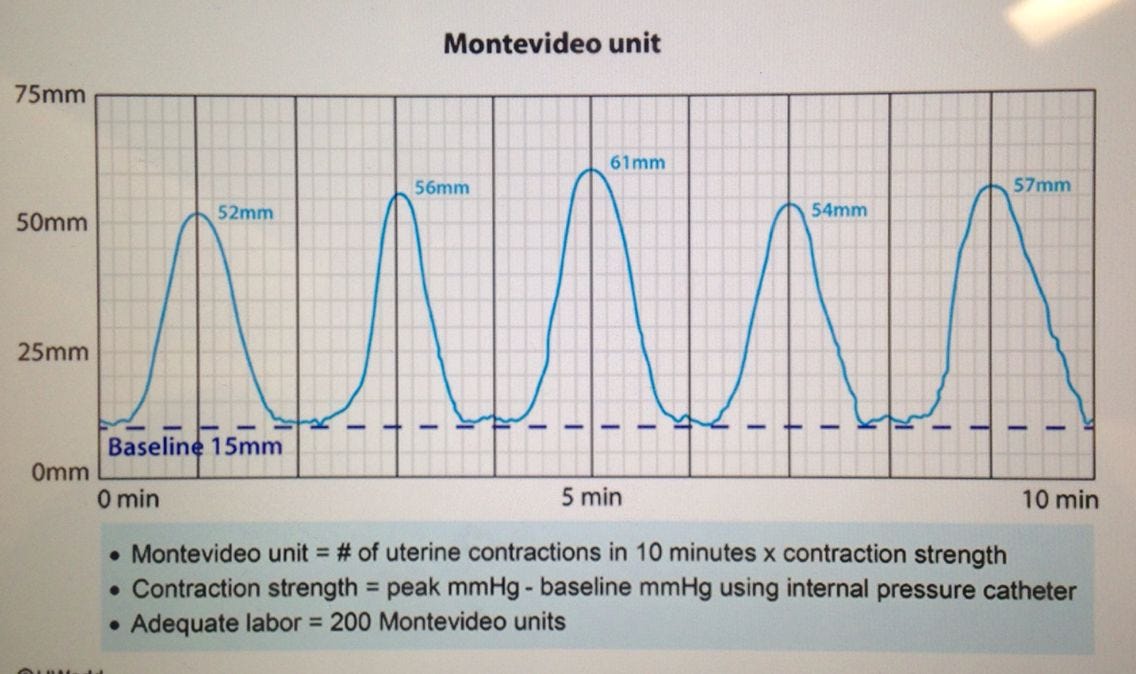
In the hospital, we start oxytocin at 1-2 milliunits/min then gradually increase it every so often with the goal of achieving 4-5 strong uterine contractions over a 10-minute interval. We can use an intrauterine pressure catheter to determine the strength of the contractions, and then we have a means of calculating the area of the curve with the goal of achieving long and strong contractions before we determine that vaginal birth isn’t going to happen. All the while, we can decrease the infusion rate by 1-2 milliunits/min (or stop it altogether) if the fetus shows distress per fetal heart rate monitoring.
Sit with this for a second. We don’t know precisely how much oxytocin is released, when its released, for how long it is released, or how much is released into the blood versus the brain, but somehow it works.
This is why many of us advocating against the willy-nilly use of Pitocin® mean when we suggest that uterine tachysystole doesn’t generally happen in the home environment. We don’t end up with as many cesareans because we aren’t rushing nor interfering with the process.
The concern for tachysystole is sufficiently high that major OBGYN journals have featured publications aimed to decreasing the cesarean rate that has resulted from a cavalier, overly aggressive use of Pitocin®. This also explains why, in 2007, intravenous Pitocin® was added to the list of high-alert medications by Institute for Safe Medication Practices (ISMP). We haven’t learned know how to use it safely…
Nature is beautiful and hard to replicate.
Beyond tachysystole
Various means of addressing this tendency for hyperstimulation of the uterus, such as checklists and protocols that have been published as much as a means of justifying ongoing induction of labor and the use of Pitocin® as a means to minimize the risk of distressing the fetus during these procedures. The attitudes of such authors were summed up in one sentence in a 2009 AJOG article: “There is no place in modern obstetric practice for ‘pitting to distress,’ ‘pitting through’ a pattern of excessive uterine activity, or continuing to blindly increase the oxytocin dose until the 1-minute Apgar score is recorded.” Aho. Amen. Àṣẹ.
But is tachysystole the only thing we must be concerned with when discussing induction or augmentation of labor.
In Part 1, I described the role of sympathetic and parasympathetic nervous systems, SNS and PNS, respectively. If you recall, I mentioned that there appears to be an inhibitory effect on oxytocin release from the pituitary when a woman is under stress, suggesting a direct influence of the SNS (“fight, flight”) on the beautiful, natural, pulsatile release of oxytocin in labor.
Those who have their babies at home utilize relaxation techniques, acupressure, soaking in warm bathtubs, calming soundtracks, and other modalities to calm the SNS, which likely supports the natural release of oxytocin, which is probably why some of these women even use words like “pleasurable” and “orgasmic” when they give birth outside of the hospital.
On the other hand, what effect might the noise, interruptions, starvation, needle sticks, questioning, and strangers in the room during hospital labor have on the SNS and thus oxytocin release? You know the answer.
Hospital clinicians are quick to offer Pitocin® augmentation when labor starts to “stall”. It’s infused continuously, and the rate is increased with time. Maybe a baby is born, maybe not.
We all have heard the moniker “healthy mom, healthy baby” in the clarification of a woman’s goals in childbirth, but perhaps the cost goes beyond a living mother and living baby?
If this is our only goal, then it’s a pretty low bar…
Too much oxytocin = downregulated receptors
Every hormone, oxytocin notwithstanding, is produced in one part of the body and travels to other parts of the body to exert its effects. It exerts it effects through a lock-and-key relationship with its receptors.
If a hormone is present continuously in large amounts, the receptors will start to disappear, making it hard for the hormone to exert its effects. This is the hallmark of insulin resistance.
With most hormones, large amounts can feedback to the gland from which it originated, resulting in less hormone being released.
Could either of these be true for oxytocin?
We have learned from animal studies that oxytocin receptors are down-regulated (“oxytocin resistance”) within 4-5 hours when administered in a continuous fashion, which explains why we have to continue to up-titrate the rate of infusion throughout an induction. And most if any is reaching the woman’s brain…
Several researchers have examined some of the important questions that are important to birthing families with relation to Pitocin® administration intra- and postpartum:
Oxytocin receptors are down-regulated through continuous exogenous infusion of Pitocin®, and re-sensitization can take hours after cessation of the infusion, meaning an increase in vagal tone, which can impact neonatal-maternal bonding and lactation, which is an issue, because breastfeeding has a known suppressive influence on the maternal SNS
When oxytocin is infused, especially at the high rates you typically see on maternity units, the brain, through negative feedback, will suppress production and release of a woman’s endogenous oxytocin. In rodent studies, “when endogenous oxytocin is genetically or pharmacologically blocked, anxiety-like and depression-like behavior increases in oxytocin-deficient knockout mice compared to wild-type mice.”
Does Pitocin® cross the placenta? Probably. The real stuff appears to transfer from mother to placenta through protein coupling, and the transfer rate is very highly controlled. And some researchers who have looked into this have cautioned against augmentation of labor, as this trending practice could have unforeseen impacts on the baby’s own oxytocin axis and response to oxytocin
Oxytocin is released into the brain and into the blood. If its release is suppressed centrally through the exogenous use of Pitocin®, this may impact the important changes in the maternal brain that support bonding with her newborn. Many other researchers have asked this question (2019, 2020), but nobody has concluded (yet) that synthetic Pitocin® which is confined to low doses due to the increased number of oxytocin receptors on the uterus in the 3rd trimester and labor impacts maternal-neonatal bonding. I’d also be remiss if I didn’t give a hat tip to Jodi Pawluski, PhD, on her work in elaborating on “mommy brain”.
Administration of synthetic oxytocin or an oxytocin receptor antagonist to primate was found to influence “optimal maternal behavior”
Endogenous oxytocin release - due to the loss of the natural endocrine rhythms that facilitate natural birth or otherwise - can be impacted by mode of delivery. Female voles who gave birth by cesarean section exhibited infanticidal behaviors compared to voles who gave birth vaginally (but also had a sham cesarean surgery)
A 2015 paper investigated concerns over a child’s risk of developing attention deficit hyperactive disorder (ADHD) and found a positive association with exposure to perinatal Pitocin® administration
Some researches are concerned that prolonged, continuous exposure to Pitocin® may be linked to autism in children
Other researchers have also taken note, suggesting that perhaps the way in which Pitocin® is infused in labor (infusion rate, continuous fashion, etc.) can lead to desensitization of newborns to their own endogenous oxytocin, which may also be partially responsible for autism spectrum disorder
An observational study published in Nature (2022) found that Pitocin® exposure in intrapartum may “affect the full expression of neonatal instinctive behavior within 2 h after birth, and adverse to the initiation and continuation of breastfeeding.”
Here is an important review paper that can provide additional insights: Bell et al, 2015.
I could continue to cherry-pick the evidence, but I won’t. The point here is that oxytocin is poorly understood, and sometimes there are downstream consequences when we become overly reliant and use too little discernment in our administration of Pitocin® in childbirth.
In conclusion…
Maybe synthetic Pitocin® is just as good as endogenous oxytocin. Maybe cesarean section isn’t increased by early IOL. Maybe we should be universally inducing everybody at 39 weeks.
We have developed the tendency to use clinical research funding to support our internal bias. In this case, the conventional medical model wants faster patient turnover in their maternity units. They want to maintain an illusion of control over a natural process. And when research is published that enables the machine to continue to make huge profits for their c-suites even it these profits come at the expense of maternal, paternal, and neonatal well-being, then those studies are going to be prioritized. This is a story that been playing out since the early 20th century.
When we pause and ask ourselves: “How could childbirth be best supported?” Most of us, regardless of our experience in caring for birthing families, are naturally going to agree that our poor maternity statistics are unlikely due to deficiencies in synthetic pharmaceutical infusions.
Most importantly, what kind of world are we creating if babies aren’t being born through love? This is hard to measure, but your heart and imagination can fill in the gaps.
Many want “proof” that the majority of interventions are problematic. To this I say: “The burden of proof lies on the interventionist.”
As we’ve learned through our legacy of attempting to manipulate and improve on nature - in land management, agriculture, and medicine - have more often than not fallen well short of any prize.
Nature nearly always wins in the face of uncertainty.

