This one pairs nicely with the 2020 Bonterra Cabernet Sauvignon (Organic)
Five Pearls
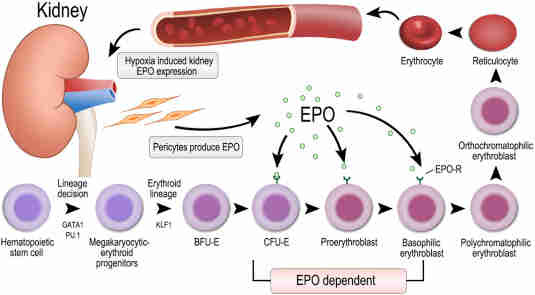
1. Normal physiologic changes in pregnancy that are relevant in anemia: blood volume expands by 50% (increased iron requirement), red blood cell mass increases by 25% in a singleton pregnancy, and increased iron stores in the female body during pregnancy help to sustain the increased demand.
2. Low serum ferritin is the most sensitive and specific single lab finding in iron deficiency anemia. And yet, it’s specificity isn’t great.
3. The CDC recommends universal screening for iron deficiency anemia in pregnancy along with universal supplementation.
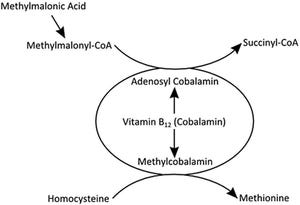
4. B12 deficiency and folate deficiency are common causes of macrocytic anemia; folate deficiency much more likely than B12.
5. Blood transfusions are almost never indicated in pregnancy, apart from the rare case of a large, concealed placental abruption (Hgb <6 g/dL is associated with abnormal fetal oxygenation --> non-reassuring fetal heart rate patterns, reduced amniotic fluid volume, fetal cerebral vasodilation, and fetal death)
Definition of anemia in pregnancy
Hgb = hemoglobin; HCT = hematocrit
- Hgb <11g/dL or HCT <33% in the first/third trimesters
- <10.5 g/dL or <32% in the second trimester
- everybody should be screened in the 1st trimester and at 24-28 weeks
- If hematocrit level is less than 33% in the first and third trimesters or less than 32% in the second trimester, you need to investigate the cause. If iron deficiency is ruled out, other etiologies should be investigated
- Living at a high altitude and tobacco use cause a generalized increase in hematocrit and hemoglobin levels, and consideration of these factors may be appropriate when interpreting test results
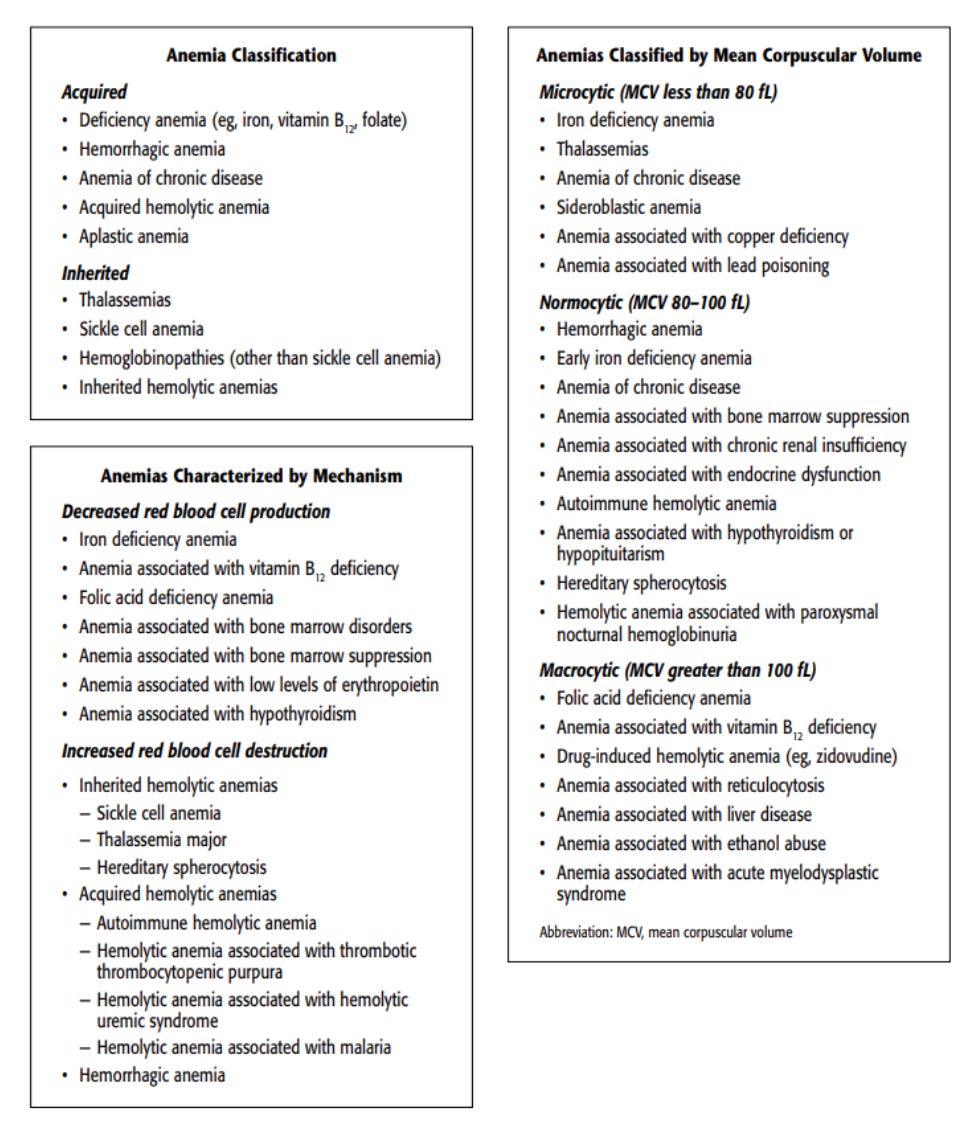
Classification of anemia
Physiologic changes in pregnancy that may lead to anemia
- blood volume expands by 40-50% (increased iron requirement)
- red blood cell mass increases by 15-25% in a singleton pregnancy
- increased iron stores in the female body during pregnancy help to sustain the increased demand
**UK guidelines on iron deficiency anemia: https://www.bsg.org.uk/wp-content/uploads/2021/09/Iron-Deficiency-Anaemia-in-Adults.pdf
“An SF level of <15 µg/L is indicative of absent iron stores, while SF levels of less than 30 µg/L are generally indicative of low body iron stores. The lower limit of normal for most laboratories, therefore, lies in the range 15–30 µg/L.”
Structure of hemoglobin
- four polypeptide chains + heme
- the six chain types: alpha (α), beta (β), gamma (γ), delta (δ), epsilon (ε), and zeta (ζ)
- adult hemoglobin consists of two alpha chains + either two β-chains (hemoglobin A), two γ-drains (hemoglobin F), or two δ-chains (hemoglobin A₂)
- hemoglobin F predominates in the developing fetus from 12 -24 wga, after which hemoglobin A begins to increase
Iron deficiency anemia
- 2% prevalence in general female population (2x higher for black women compared to white)
- “An assessment of iron status in pregnant individuals in the United States using data from the National Health and Nutrition Examination Survey (known as NHANES) from 1999 to 2006 found that iron deficiency prevalence increased significantly with each trimester (mean ± standard error, 7%, 14%, and 30%, in the first, second, and third trimesters, respectively) and was higher in Mexican American pregnant women, non-Hispanic Black pregnant women, and women with parity greater than 2”
- in pregnancy, higher prevalence by far in 3rd trimester
- associated with low birth weight, preterm delivery, and perinatal mortality
- there may also be an association with postpartum depression and worse mental and psychomotor performance testing in offspring
- diagnosed by lab analysis OR if there's an increase in Hgb by 1g/dL after iron treatment OR by the absence of bone marrow iron stores on bone marrow biopsies
- iron storage may be low (iron depletion), or stored + transport iron are low (decreased erythropoiesis), or stored + transport + functional iron are all low (full blown iron deficiency anemia, yeehaw!)
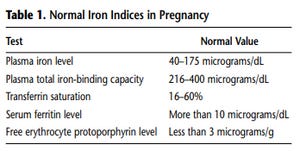
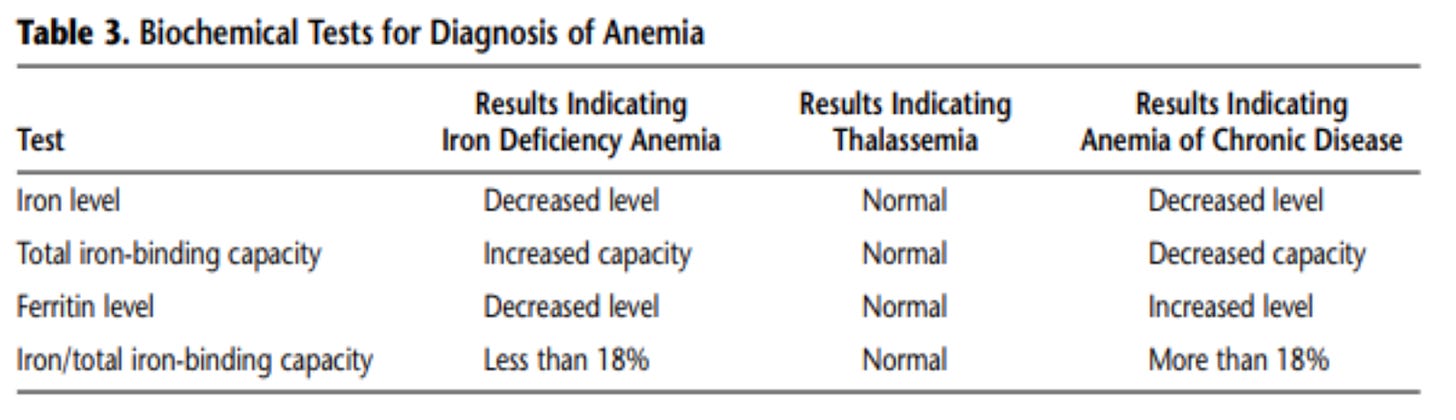
- on iron studies, iron deficiency anemia presents as: microcytic, hypochromic, iron store depletion, low plasma iron, increased total iron-binding capacity (TIBC), low serum ferritin, and increased free erythrocyte protoporphyrin
- serum ferritin levels are most specific and sensitive for the diagnosis (<10-15 mcg/L is diagnostic)
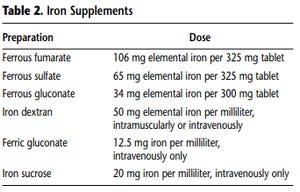
- CDC recommends universal screening of pregnant women along with universal supplementation (unless the patient has hemochromatosis)
- typical American diet provide 15 mg of elemental iron per day (recommended: 27 mg daily iron intake)
- extended-release formulations are less effective
- foods rich in iron: shellfish, beef, organ meats, turkey, beans, and lentils
- foods that enhance iron absorption from the gut: citrus, strawberries, broccoli, and peppers
- foods that impair iron absorption: dairy, soy, spinach, and coffee
Macrocytic anemia
- two general categories: megaloblastic (B12 or folate deficiency, pernicious anemia) and non-megaloblastic (liver disease, myelodysplasia, increased reticulocytes, aplastic anemia, and hypothyroidism)
- mean corpuscular volume (MCV) >100 fL is characteristic of macrocytic anemia
- if >115 fL, diagnostic for folate acid or B12 deficiency (confirm by checking serum folate acid or B12 levels)
- in the U.S., macrocytic anemia in pregnancy is due almost exclusively to folate deficiency
- recall: folic acid should universally be supplemented at 400 mcg per day in pregnancy
- however: 40-60% of the U.S. population carries of a variant of a mutation within the gene that encodes for the MTHFR enzyme, and folic acid is useless in that case
More on folic acid versus folate from Lily Nichols, RDN
- folate deficiency can be caused by diets deficient in leafy vegetables, legumes, or animal proteins (or taking antacids) - changing the diet should do the trick (you can also increased folic acid supplementation to 1 mg daily along with increasing iron supplementation)
- B12 deficiency can be seen in women who have undergone partial or total gastric resection or in Crohn disease
- treatment includes supplementing with 1000 mcg of B12 (intramuscular) monthly
What if a patient has laboratory evidence of anemia but is asymptomatic?
- mild: reasonable to investigate further through iron studies, RBC indices, etc. (otherwise you may just recommended dietary changes without investigation)
- moderate: definitely investigate the etiology (CBC, RBC indices, iron studies, blood smear), consider Hgb electrophoresis if patient is of African, Southeast Asian, or Mediterranean descent; reasonable to treat empirically with iron while awaiting further studies (you should see results in a few weeks)
When should transfusion be considered?
- almost never in pregnancy, apart from the rare case of a large, concealed placental abruption (Hgb <6 g/dL is associated with abnormal fetal oxygenation --> non-reassuring fetal heart rate patterns, reduced amniotic fluid volume, fetal cerebral vasodilation, and fetal death)
- postpartum is a different story: coagulopathy (HELLP, DIC, etc.), uterine atony, placenta previa/accreta, and placental abruption may all result in the need for transfusion postpartum
- if the patient becomes symptomatic or hemodynamically unstable then it's a no-brainer
When should iron infusion be considered?
- useful for the rare patient who can't tolerate oral iron or those who have severe malabsorption issues
- 1% chance of anaphylaxis (iron dextran more likely to cause a reaction than ferrous sucrose)
- faster immediate results from IV iron compared to oral for most patients, but by day 40 after treatment, the two routes of comparable
- insufficient data to guide decisions around erythropoietin treatment in pregnancy
My approach:
Evaluate for all potential causes of anemia before treatment (Ready —> Aim —> Fire; Not the other way around). Often iron deficiency plays a role, but rarely is it just about iron.
Instead of repleting iron willy-nilly, try to determine if absorption is the underlying issue. Adding acids like apple cider vinegar or HCL capsules to the diet can help with reabsorption. Calcium-rich foods can impede absorption. You can bet that absorption is at least partially responsible if ferritin is low, although ferritin itself is wildly misunderstood (including by me). For example, there is little if any iron found in a molecule of ferritin, so what’s the deal? Well, while ferritin reflects overall “iron stores”, this association is more likely indirect. Ferritin is more likely a powerful antioxidant. My clinical experience tells me that iron deficiency anemia will at least be partially corrected for (with improved outcomes) if low ferritin is managed by focusing on absorption of iron. Bear in mind, also, that the antioxidant response element, which is regulated by Nrf2, a master gene in the regulation of our response to oxidative stress, regulates the expression of the gene that is responsible for ferritin production, meaning foods and supplements meant to regulate Nrf2 can also have an impact on ferritin levels. Note: this means foods and supplements that flood the body with antioxidants may be impactful to iron storage and utilization, but, again, I haven’t figured this out entirely. But others are also asking these questions…
I always aim for a serum ferritin level of at least 50 ng/mL
Adequate nourishment through whole foods, namely beef liver, bivalves like oysters, bone broth, fermented cod liver oil, and farm-fresh eggs are all helpful for the increased demand on RBC production. There’s no question about this. You’ll have adequate amounts of folate (Vitamin B9), other B vitamins, fat-soluble vitamins, Omega 3s, Cu/Zn, Se, Mg, and other nutrients critical for healthy absorption, transport, and storage of iron (and general health before, during, and after pregnancy).
I don’t generally recommend supplemental iron, as you’ll get more bang for your buck (and avoid constipation) by striving to acquire these nutrients from whole food sources.
Address underlying inflammation, which can be tricky to identify while in pregnant state, which is, in some regards, an inflammatory state in and of itself.
We could go much deeper…but for the every day practitioner, this is hopefully a good start.
Notes for this episode are found on Substack.
Questions? Leave a comment.
Work with Nathan:
Beloved Holistics | Born Free Method | Clear & Free | Twins-Breech
Medical Disclaimer: Born Free Method: The Podcast is an educational program. No information conveyed through this podcast should be construed as medical advice. These conversations are available to the public for educational and entertainment purposes only.
Music provided by AudioKraken / Pond5













Share this post