Pairs well with the 2021 Russian River Pinot Noir Davis Family Vineyards
Five Pearls
1. Cell-free DNA screening has the best sensitivity and specificity of all screening methods. But before you order it, it's best to get a prenatal ultrasound
2. Best non-cell-free screening modality is the sequential integrated serum screen (1st-tri serum + NT ultrasound + 2nd-tri serum)
3. Formal anatomy survey should be offered at 18 - 22 wga; can identify soft markers for T21 and T18
4. Prenatal genetic screening should be offered to all pregnant women regardless of risk profile
5. Anything that doesn't add up, it's best to just refer to a genetics counselor or even your friendly MFM for clarification.
The (very) Basics of DNA and Reproduction
apart from RBCs and cornified cells of your skin, hair, and nails, every one of your body's cells has a nucleus
gametes (sperm or ova) are haploid, meaning their nuclei contain 23 chromosome
somatic cells are diploid, meaning their nuclei contain 23 pairs of chromosomes (46 chromosomes total)
when a sperm meets an ovum, magic happens!
the sperm fertilizes the egg to create a zygote: the 23 chromosomes of the sperm combine with the 23 chromosomes of the ovum
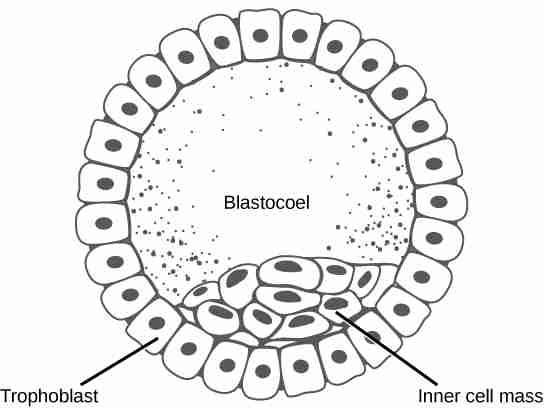
for the next 24 hrs, the zygote undergoes rapid, mitotic division ("cleavage"); after about 100 cells have been formed, it's called a blastula
the total mass of the original zygote has not changed, it has merely divided, and each individual cell is called a blastomere
the blastula consists of a spherical layer of cells called the blastoderm surrounding a yolk-filled cavity called a blastocoel.
in mammals, the blastoderm arranges itself into an inner and outer layer of cells, the embryoblast and trophoblast, respectively. The former will go on to form the fetus, the latter the placenta.
Illustration credited to Libretexts.org (click image for source)
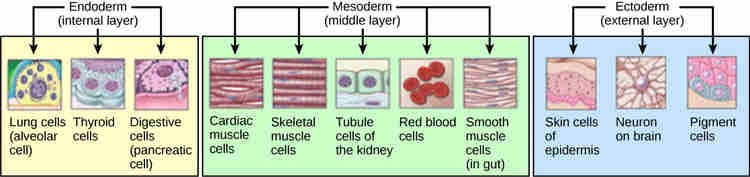
the embryoblast undergoes gastrulation, where it rearranges itself into three germ layers: endoderm, mesoderm, and ectoderm, and the fetus gradually develops from here
any chromosomal defect - whether parts missing, extra copies, or missing copies - can lead to abnormalities in the development of the fetus
Illustration credited to Libretexts.org (click image for source)
Epidemiology of chromosomal abnormalities
chromosomal abnormalities are found in 1-in-150 pregnancies
they are more common in the 1st trimester (aneuploidies are the most common reason for early pregnancy loss)
incidence of aneuploidies increases proportionately with maternal age and presence of a paternal chromosomal abnormality or translocation
Trisomy 21 (Down syndrome) is the most common chromosomal aneuploidy among live infants (1-in-700 live births)
although risk of aneuploidies correlates w/ maternal age, most T21 kids are born to young women because overall, young women have more children than older women
Trisomy 18 (Edward syndrome) is the 2nd most common (1-in-3000)
Trisomy 13 (Patau syndrome) is the 3rd most common (1-in-6000)
the most common sex chromosome aneuploidy is 47, XXY (Klinefelter syndrome), which is seen in 1-in-500 males
the only viable monosomy is 45, X (Turner syndrome), which is seen in 1-in-2500 females and is unrelated to maternal age
unlike aneuploidies, copy number variants are independent of maternal age
a copy number variation is a type of duplication or deletion event that affects a considerable number of base pairs within a chromosome; it can be detected on microarray
in pregnancies where the mom is age 36 or less, microarray abnormalities are more common than aneuploidies
prenatal genetic screening should be offered to all pregnant women
if a screen is positive, diagnostic testing should be offered
Single time point screening approaches
Cell-free DNA screening
can be used as early as 9-10 wga
can detect sex of fetus
genetic material is found in maternal circulation
derived from placental trophoblasts
in pregnancy, of the cell-free DNA found in maternal circulation, 3-13% is fetal in origin (increases as pregnancy advances)
most sensitive and specific for common aneuploidies
sex chromosome results for patients who have undergone organ transplant will be affected by the sex of the organ donor so not recommended for these patients
overall best screen: 98-99% sensitivity for T21, T18, T13; 0.13% combined false positive rate (also extremely low false negative rate)
before you send a cell-free DNA screening, best to get a prenatal ultrasound to (1) confirm dating, (2) detect obvious fetal anomaly, (3) detect presence of multi-gestation pregnancy, and (4) confirm viability, any of which can influence cell-free DNA screening results
if the final result is: "no result reportable" or "results uninterpretable", the pregnancy is at higher risk for chromosomal abnormalities
can detect some microdeletions, less common aneuploidies like T16 and T22, and large copy changes but false positive rates haven't been established (if any of these are detected, refer for diagnostics)
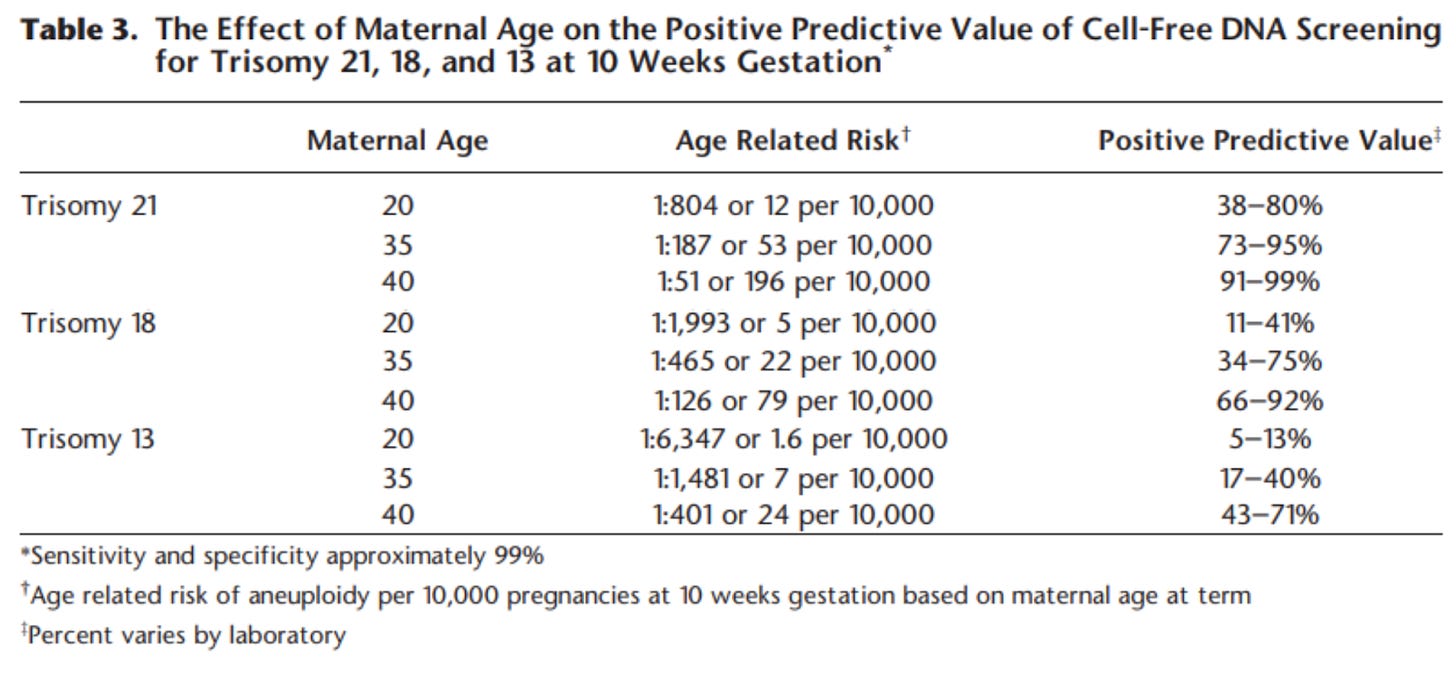
lower PPV rate in younger patients given that fetal chromosomal abnormalities are less prevalent in younger patients (Table 3)
First-trimester screening
Credit to The Fetal Medicine Foundation
most accurate at 10 - 14 wga (38 - 84 mm CRL)
includes nuchal translucency (NT) ultrasound and serum biomarkers (PAPP-A, and hCG)
PAPP-A = pregnancy associated plasma protein A
hCG = human chorionic gonadotropin
these values are used in conjunction with maternal age, weight, race, number of fetuses, and history of aneuploidy to create a composite likelihood score of common trisomies (T21, T18, and T13) (see Table 2)
NT ≥ 3mm is an independent risk factor for fetal aneuploidies and fetal cardiac defects
NT ultrasound alone
NT alone detects 70% of aneuploidies
adds nothing of use to cell-free DNA screening in a singleton gestation
more on first-trimester ultrasound below
Fetal anatomic survey
offered at 18 - 22 wga
full head to toe ultrasound assessment of the fetal anatomy
offered to all patients regardless of decisions around 1st or 2nd trimester screening
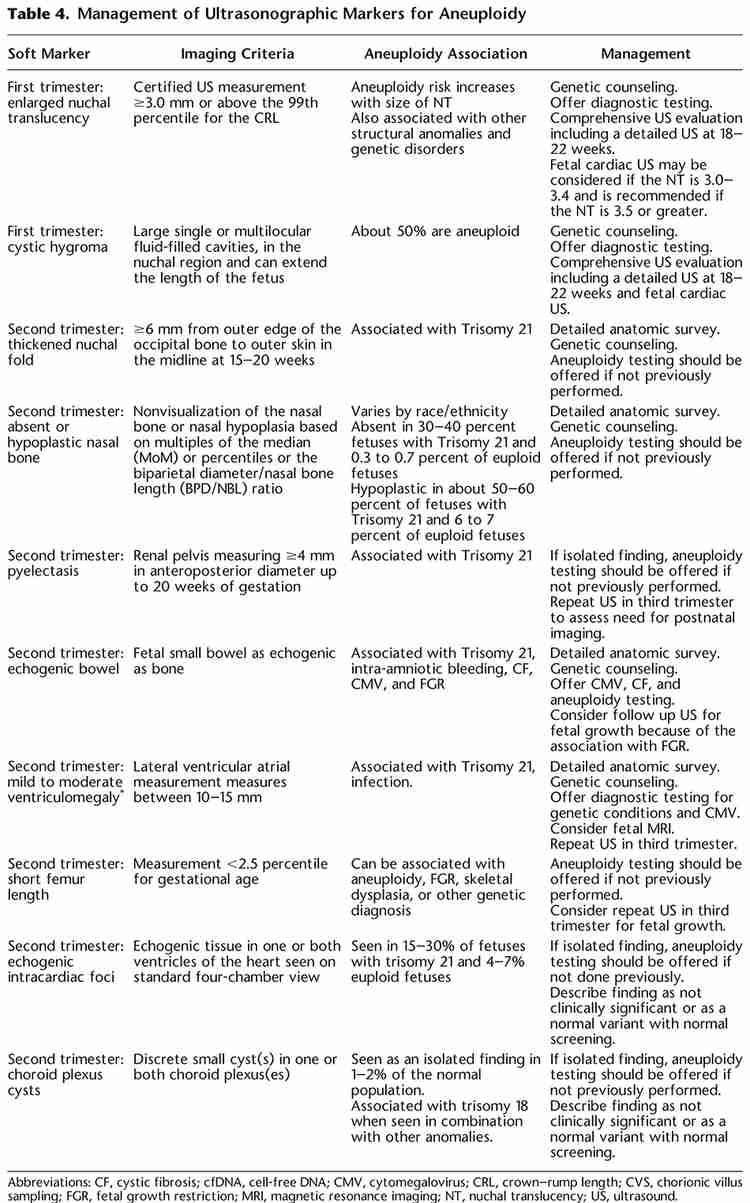
can identify soft markers for T21 (echogenic intracardiac focus, thickened nuchal fold, renal pelvis dilation, and echogenic bowel) and T18 (choroid plexus cysts)
T18 and T13 are likely going to have major structural anomalies notable on ultrasound; 27% of T21 fetuses will have major anomalies
Second-trimester screening
"Quad screen": hCG, dimeric inhibin A (DIA), unconjugated estriol (ue3), and alpha fetoprotein (AFP)
offered b/w 15 - 22w6d
composite score (along w/ maternal data) provides likelihood for T21, T18, and neural tube defects (see Table 2)
some labs offer a triple screen (quad screen without inhibin), but it's not as effective and more costly than the quad so don't bother
Combined first- and second-trimester screening
combines first-trimester serum screening, NT ultrasound, and second-trimester serum screening, which improves overall accuracy and detection rates (see Table 2)
Integrated screening
first-trimester serum screen, NT ultrasound, and second-trimester serum screen performed and a final score is given at the end
if NT ultrasound not available, lower detection rate than if NT ultrasound were included, but similar detection rate of first trimester screening
Sequential and contingent screening
same as integrated, but a score is given after the first-trimester screening so that diagnostics can be provided earlier rather than waiting until after second-trimester screening if risk of aneuploidy or neural tube defect is sufficiently high to warrant further investigation
diagnostics would consist of CVS or amniocentesis depending on timing, though often preceded by cell-free DNA screening
How should women be counseled about the risk for fetal chromosomal abnormalities?
use Table 1 to give your patient information about their risk of fetal chromosomal abnormalities based on age, history of prior pregnancies affected by fetal chromosomal abnormalities, and their personal and family genetic history
review all screening methods
don't do both cell-free DNA screening and integrated/sequential screening simultaneously as it's not cost effective and you won't know what to do with discordant results
What if my patient's screen is positive?
well first, remember that screens are not diagnostic tests
give them the composite risk of chromosomal abnormality
false positives on cell-free DNA screening are more rare than other screening methods, but can be seen in the event of mosaicism (presence of normal and abnormal cells in the fetus), maternal malignancy, a duplicated chromosomal region, or in vanishing twin syndrome
refer for diagnostic testing if patient desires to know for sure
even if cell-free DNA screening suggests aneuploidy, diagnostics will help determine if its a trisomy or translocation (important because a translocation can come from either parent and can be passed to future generations)
consider how this information might be important to them
What if my patient's screen is negative?
pretty great chance that there is no fetal chromosomal abnormality, but nothing in pregnancy is guaranteed
diagnostic testing can still be offered if patient is concerned, particularly if new findings emerge as pregnancy progresses
cell-free DNA screening has extremely low false negative rate, but can result from mosaicism, low fetal fraction (if performed at <9 wga), and lab error
you could offer repeat cell-free DNA screening, but this might delay diagnostics; if ultrasound findings are consistent with chromosomal abnormality, it's probably best to go to diagnostics
More on first-trimester ultrasound
absence of nasal bone is also a marker for aneuploidy (49% sensitivity, 1% false positive rate)
increased NT is associated with genetic syndromes along with anomalies like cardiac defects, abdominal wall defects, and diaphragmatic hernia (even if normal chromosomes found on diagnostic testing)
if NT is increased along length of fetal spine, this is called a cystic hygroma (55% will have abnormal karyotype like T21, monosomy X, and T18); if karyotype normal, 30% will have a major congenital anomaly (e.g. cardiac, urinary, and CNS)
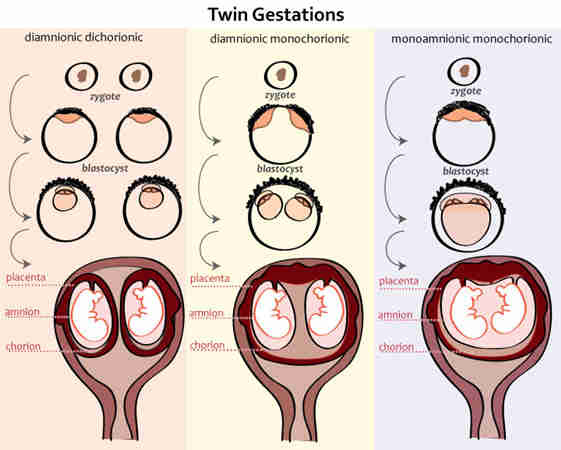
How to screen for fetal chromosomal abnormalities in twin gestation pregnancy?
none of the screening methods are as predictive in twin pregnancy
think about it: dizygotic twins are more common, and they have different genetic makeup
even monozygotic twins with discordant karyotype have been described
combined first-trimester screening (for twins) will detect 90% of fetuses with T21 (5% false positive)
NT ultrasound is just as useful in twin gestations compared to singleton
Should patients who underwent IVF accompanied by pre-implantation genetic testing still consider screening?
in theory, there's no benefit, but we don't have enough data to guide this decision
lab errors and false negatives happen
What other information about the pregnancy can be gleaned from screening for fetal chromosomal abnormalities?
low or high fetal fraction on cell-free DNA screening is independently associated with adverse pregnancy outcomes related to placental dysfunction and hypertensive disease
low PAPP-A on first-trimester serum screen is associated with higher risk of SAB, IUFD, neonatal demise, growth restriction, preterm birth, placental abruption, and preeclampsia
elevated AFP, DIA, or hCG on second-trimester serum screen is associated with high risk for IUFD, growth restriction, and preeclampsia
all poor PPV, though, so not reliable alone as screening tests for these outcomes
Also mentioned in the podcast:
My favorite prenatal vitamin: Wenatal (free fish oil with this link!)
My men’s intimacy coach, Ted Riter
Zoom link for information session on a special opportunity in collaboration with Maryn Azoff of Vocal Transformation. (Mark your calendar! October 30th, 7:30pm ET!)
Notes for this episode are found on Substack.
Work with Nathan:
Beloved Holistics | Born Free Method | Clear & Free | Twins-Breech
Medical Disclaimer: Born Free Method: The Podcast is an educational program. No information conveyed through this podcast should be construed as medical advice. These conversations are available to the public for educational and entertainment purposes only.
Music provided by AudioKraken / Pond5

















Share this post