I paired this episode with the 2021 Pinot Noir from Imagery.
Five Pearls
Prevention is key. Work on modifying lifestyle well before conception for best outcomes
Sugar is toxic as hell to our vital organs, and our growing baby/placenta are no exception.
Insulin appears to be associated with the best outcomes compared to oral agents.
C-section for suspected fetal macrosomia is for the birds.
Inducing a woman with well-controlled GDM probably isn’t always in her best interest.
Epidemiology
7% of pregnancies are impacted by any type of diabetes
86% of those impacted are the result of GDM
Compared to all other ethnicities, white women are impacted the least
Older age at time of conception, sedentary lifestyle, and pre-pregnancy obesity are risk factors (same risk factors for type 2 DM outside of pregnancy)
Maternal complications
9.8% chance of developing preeclampsia when fasting blood sugar is <115 mg/dL
18% change of developing preeclampsia when fasting blood sugar is >/= 115 mg/dL
17% chance of undergoing c-section with diet-controlled GDM versus 25% if medication is required (9.5% without GDM)
70% of women who develop GDM will develop type 2 DM within 22-28 years after pregnancy, but this varies by ethnicity (60% of hispanic women who develop GDM will develop type 2 DM within 5 years of pregnancy)
Fetal/neonatal complications
Increased risk macrosomia, neonatal hypoglycemia, hyperbilirubinemia, shoulder dystocia, and birth trauma
Several agencies have cautioned around the risk of stillbirth, as well, but the data for this is poor at best. Rachel Reed recently wrote a nice blog (rant) about the topic in her newsletter
Linear relationship between any abnormal value on the 2-hr 75-g OGTT and c-section, birth weight >90th percentile, neonatal hypoglycemia, and fetal hyperinsulinemia
Higher risk of your child developing type 2 DM in their lifetime
When did GDM screening arise? 1963
This study was undertaken to: “evaluate various methods of screening for the ‘prediabetic state’ which often becomes recognizable during pregnancy.” - Wilkerson et al, 1963
Screening strategies:
1st trimester: reasonable if there are risk factors or if you live in a city/region with high prevalence
50-g oral glucose challenge (non-fasted) (two-step)
If negative, repeat at 24-28 weeks
If positive (>130-140 mg/dL), move to 3-hr oral glucose tolerance test (see below)
Straight to a 75-g oral 2-hr glucose tolerance test) (one-step)
Check fasting sugar → drink the drink —> check blood sugar at 1 hr and 2 hr
If either value is elevated, then you have your diagnosis
HgA1C: potentially insightful in 1st trimester but not as sensitive as oral glucose challenge/tolerance test
24-28 weeks: reasonable to defer in 1st trimester if low prevalence community or minimal risk (and no need to repeat if diagnosed in 1st trimester)
Same options as above
If 1-hr OGC was elevated in 1st trimester, but 3-hr OGTT was negative, you can simply repeat the 3-hr OGTT (100 g bolus) without repeating the 1-hr OGC
3-hr OGTT (100 g)
Checking fasting blood sugar → drink the drink → check blood sugar after 1, 2, and 3 hrs
2 of 4 values elevated is consistent with diagnosis (although some have argued that 1 value is sufficient):
“Although a higher level of scrutiny may be focused on this subset of women, further research is needed to clarify the risk of adverse outcomes in patients with one abnormal value on the 100-g, 3-hour OGTT and whether they would benefit from treatment.”
Glucola has a bunch of junk in it. Fingersticks and CGM are very reasonable alternatives to the sugary drink. Orange flavor from Fischer-Scientific contains artificial food dyes that don’t belong in the human body, especially when growing a baby. If an oral glucose test is preferred, consider Fresh Test instead of Glucola. There is no data to support gummy bears, fruit juice, or any other alternatives.
What are some of the risk factors that might prompt early screening:
Benefits of treatment
2005 study out of Australia found that treatment of GDM resulted in less:
Serious newborn complications (composite of perinatal death, shoulder dystocia, and birth trauma, including fracture or nerve palsy)
Preeclampsia (from 18% down to 12%)
Less large for gestational age (LGA) infants (from 22% down to 13%)
Less risk of birth weight being >4000 g (from 21% down to 10%)
2009 study out of the US found that treatment of “mild” GDM resulted in less: hypertensive disorders, c-section, LGA infants, less babies >4000 g, reduced infant fat mass, and shoulder dystocia (but no difference in their serious newborn complication composite)
Treatment strategy
Even ACOG agrees that nutritional and lifestyle counseling is the first line of therapy:
Having said this, I’m not going to reiterate a single ounce of language in ACOG’s PB regarding “how to live a healthy lifestyle” because OBGYNs and those who treatment the Green Journal as the Bible of OBGYN are unhealthy themselves and generally have no idea what they’re talking about
Instead, please refer to the work of Lily Nichols (“Real Food for Gestational Diabetes”)
The gist:
If you are sleeping and recovering well (8+ hours per night), then go hard in the gym
If you aren’t, then focus on restorative yoga, long walks, etc., because regular movement is critical
Increase protein and healthy fats (lose the seed oils and fried food), decreased processed junk
Add in beef liver, eggs, bone broth, bivalves (like smoked oysters), and a quality fish oil (preferably cod liver oil)
Take a walk after your meal
Limit feeding window without decreasing total calories (ex: 8am to 6pm)
Stress mitigation and setting up healthy emotional boundaries
Green tea and cinnamon is easily accessible “foods” to help improve blood sugars
We must take into account socioeconomics, racism, and other structural means of chronic stress that also impact blood sugar levels through the actions of cortisol
Oral medication and insulin are often required after adequate efforts to improve lifestyle
Whichever approach, monitoring blood sugars is important throughout pregnancy (and postpartum)
Postprandial blood sugar goal:
1 hr: <140 mg/dL
2 hr: <120 mg/dL
Fasting blood sugar goal: <95 mg/dL
Review values weekly if unstable, every 2 weeks if stable
Oral medication overview
Glyburide:
Not FDA approved for glycemic control in pregnancy
Pregnancy category C
Increases insulin production from the pancreatic beta cells
2.5-20 mg daily in divided doses
Crosses the placenta (little data on potential for teratogenicity)
Less expensive and less annoying than insulin
Metformin:
Not FDA approved for glycemic control in pregnancy
Pregnancy category B
Inhibits gluconeogenesis by the liver
Increases peripheral tissue sensitivity to insulin
Historically used for women with pregestational diabetes or in women with infertility due to PCOS, and they are entering pregnancy already well-controlled through metformin
Crosses the placenta, and there is some concern around potentially teratogenic effects (though this hasn’t seemed to pan out over time)
Started at 500 mg daily for 1 week, then increased to 500 mg BID, etc. (max dose 2500-3000 mg daily)
Careful with kidney disease/insufficiency
Less expensive and less annoying than insulin
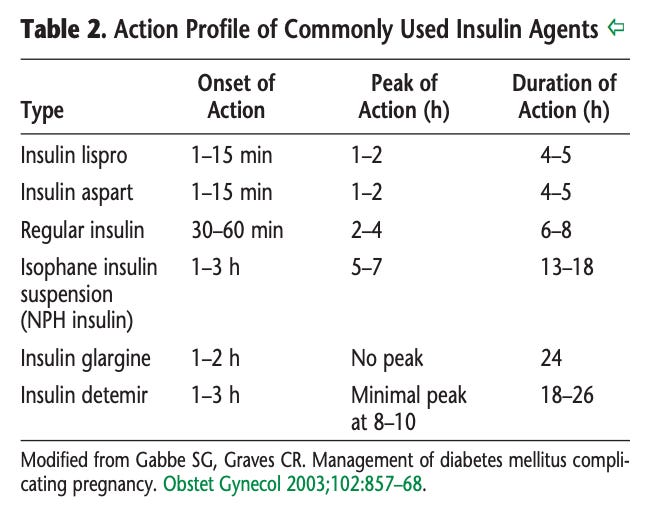
Insulin overview
Approved by FDA (and preferred by ACOG and the ADA)
Doesn’t cross the placenta
Dose of 0.7-1.0 units/kg daily is sufficient for most women, split between long- and short-acting insulin
Long/intermediate-acting: NPH is most common, but glargine and detemir re on the rise
Can be used in the AM or PM or both (BID)
Short-acting: lispro and aspart are easily accessible and have faster onset of action than “regular insulin”
best if used at time of meal (not 15 min before)
Selecting a medication
Insulin versus glyburide versus metformin?
2014 study that randomized 751 women to metformin (+insulin if needed) to insulin found no difference
2013 study compared metformin against insulin ruled in favor of metformin
Meta-analyses in 2015 and 2014: minimal difference in maternal or neonatal outcomes, but the latter found lower rates of gHTN and higher rates of preterm birth in metformin group
2017 systematic review and meta-analysis: no obvious difference
2017 systematic review and meta-analysis comparing metformin against insulin found metformin to be “non-inferior”
Some observational studies have reported higher rates of neonatal hypoglycemia and higher rates of fetal macrosomia
2017 Cochrane did a meta-analysis comparing insulin against any oral agent and concluded no significant differences
I hope you get the point…there has been a lot of effort to determine which is better
But there was a massive meta-analysis in 2021 that provides perhaps the best comparison (“the one to rule them all”)
In summary: insulin is probably best. Metformin probably 2nd best. Glyburide last.
Antepartum surveillance in GDM
Weekly or twice weekly NSTs are recommended for any woman requiring medication to manage their GDM starting at 32 weeks (earlier if other issues arise)
Diet-controlled GDM is not associated with risk of stillbirth before 40 weeks, so NSTs aren’t universally recommended, but, if they do start, you can probably wait until later in the 3rd trimester (no consensus)
Because polyhydramnios is associated with poor glycemic control, it has become relatively routine to measure amniotic fluid at the time of NST
If glycemic control has been an issue throughout pregnancy, growth ultrasound should be considered, especially if indicated by fundal height >2-3+ cm beyond gestational age
Timing of delivery
ACOG doesn’t recommend delivery before 39 weeks even if a woman is on medication
Induction at 38 weeks hasn’t been found to lower c-section rates (1993 randomized trial)
Induction at 38-39 weeks hasn’t been found to lower risk of macrosomia (or c-section) (1996 study)
Induction at 38-39 weeks has been found to lower risk of shoulder dystocia (10% versus 1.4%) when compared to expectant management (2009 systematic review)
Induction before 40 weeks has been found to lower risk of c-section (2016 study)
A decisional analysis from 2014 found that induction at 38-39 weeks results in reduced perinatal mortality without increasing risk of c-section
ACOG’s conclusion: delivery should be recommended at 39-39w6d gestation, but they aren’t the final trump card:
“In contrast, expert opinion has supported earlier delivery for women with poorly controlled GDM. But clear guidance about the degree of glycemic control that necessitates earlier delivery is lacking, and the recommendations about timing of delivery lack specific guidance as well. In light of this, consideration of timing should incorporate tradeoffs between the risks of prematurity and the ongoing risks of stillbirth. In such a setting, delivery between 37 0/7 weeks and 38 6/7 weeks of gestation may be justified, but delivery in the late preterm period from 34 0/7 weeks to 36 6/7 weeks of gestation should be reserved for those women who fail in-hospital attempts to improve glycemic control or who have abnormal antepartum fetal testing.”
What about c-section for big babies?
The idea here is that in GDM, babies tend to accumulate fat in their upper trunchal regions and thus are more susceptible to shoulder dystocia and brachial plexus injury (this is true)
However, we are notoriously inaccurate at assessing fetal weight in the 3rd trimester via ultrasound
“...data are insufficient to determine whether cesarean delivery should be performed to reduce the risk of birth trauma in cases of suspected macrosomia.”
NNT = 588 c-sections to prevent a single permanent brachial plexus injury for babies with EFW 4500 g
NNT = 962 c-sections to prevent such an injury to a baby with EFW of 4000 g
NNT means “number needed to treat”
And yet, despite this, ACOG maintains that: “it appears reasonable to recommend that women with GDM should be counseled regarding the risks and benefits of a scheduled cesarean delivery when the estimated fetal weight is 4,500 g or more”
Ideal serum blood sugar in labor/delivery
70-125 mg/dL is the goal
Postpartum management of GDM
75-g 2-hr OGTT is recommended 4-12 weeks postpartum
Up to ⅓ of women will have a positive test postpartum
7-fold increased risk of developing type 2 DM after a pregnancy complicated by GDM
Also screen for depression, as GDM is a risk factor for postpartum depression (Edinburgh Postnatal Depression Scale)
And immediately postpartum, medication dosages will likely need to be adjusted, but check blood sugars to guide these adjustments
Notes for this episode are found on Substack.
Questions? Leave a comment.
Work with Nathan:
Beloved Holistics | Born Free Method | Clear & Free | Twins-Breech
Medical Disclaimer: Born Free Method: The Podcast is an educational program. No information conveyed through this podcast should be construed as medical advice. These conversations are available to the public for educational and entertainment purposes only.
Music provided by AudioKraken / Pond5


















Share this post